Posts Tagged ‘Community’
Nicole – Pandemic’s Effect on Grieving as a Community
Nicole – Pandemic’s Effect on Grieving as a Community
Nicole discusses the ways the pandemic has affected the way people grieve as a community.
Nicole – Working in Community Outreach
Nicole – Working in Community Outreach
Nicole discusses her work in community outreach and how she has lived experience with addiction and living rough.
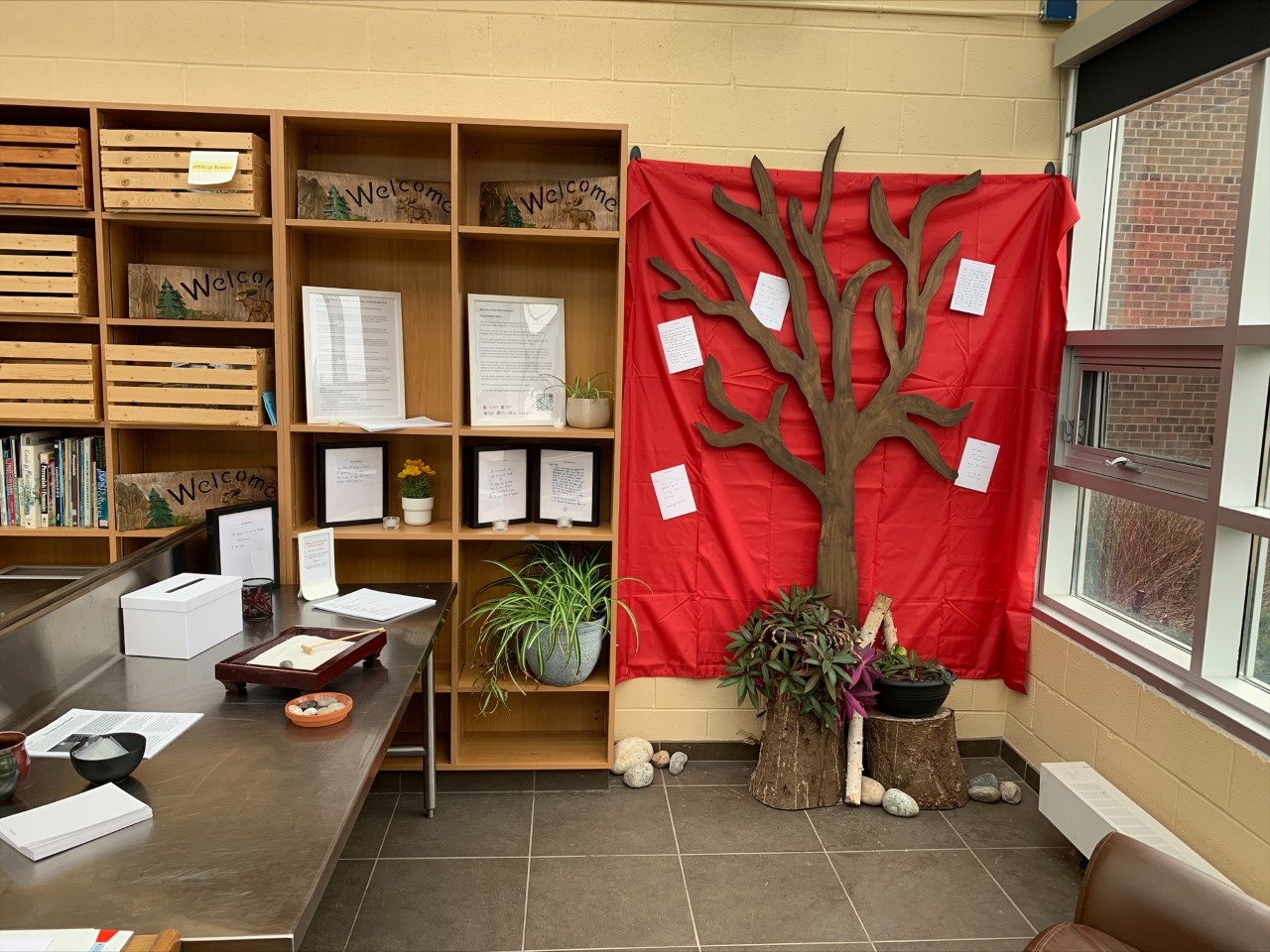
The Reflection Room® project: How storytelling supports processing grief
The Saint Elizabeth Foundation offers a project called the Reflection Room – a space for thinking and talking about dying, death, and grief.
The Reflection Room project is an evidence-based participatory art installation that was developed by researchers at the SE Research Centre and Memorial University in 2016. The project included a research component that evaluated the impact of Reflection Rooms as the project adapted over time to address changing needs.
The Reflection Room project was first developed to support people in community and healthcare settings to move from death-denying to death-discussing. From the first installation, the Reflection Room project has gone through three Phases of adaptation and continues to evolve.
Common elements across Reflection Rooms, whether they are set up to include an entire room, hallway, or corner of a room, include a quiet, calming space that invites visitors to read other people’s stories and post their own. The rooms are unstructured and unfacilitated, allowing visitors to engage with the space however they wish.
Over a five-year period from 2016-2020, the Reflection Room project was installed in 62 places across Canada, including in conferences, art galleries, hospices, and hospitals (Phases 1 and 2). Over a thousand stories were shared by individuals during their visits to these various Reflection Rooms. Results from the study from this period showed that storytelling can be an important part of grieving.
In 2020, Phase 3 of its adaptation and evaluation began with the SE Research Centre being asked to expand the reach of the Reflection Room to long-term care home communities in Ontario to respond to some of the accumulated pandemic-related grief in those communities. With the support of the Saint Elizabeth Foundation, Ontario Health Central, Family Councils Ontario, Ontario Centres for Learning, Research and Innovation in Long-Term Care, and Ontario Association of Residents’ Councils, over 50 homes signed up to host a Reflection Room®. In order to adapt to the environment of long-term care homes, an easy-to-set-up ‘kit’ incorporating instructions and materials (e.g., Reflection Cards, a red curtain to display Reflection Cards, candles, etc.) was developed and sent to homes free of cost. Overwhelmingly positive feedback has demonstrated that the Rooms support communities to work through grief by having a quiet space to rest and reflect, disclose emotions, process thoughts, and feel connected to others through sharing stories. The project often is complementary to other existing initiatives in long-term care homes such as palliative care committees and spiritual programs.
A collection of the stories shared over the course of the project is available to view on the Reflection Room website.
If you want to learn more about the project, contact foundation@sehc.com and listen to the Grief Stories podcast episode 64.
Neeliya Paripooranam, MSc, is a Project and Communications Manager at the SE Research Centre, overseeing the Reflection Room® project. Celina Carter, RN PhD, is a Senior Research Associate at the SE Research Centre. Paul Holyoke, PhD, is the Vice President, Research and Innovation at SE Health. Justine Giosa, PhD, is the Scientific Director, SE Research Centre and Adjunct Assistant Professor in the School of Public Health Sciences at the University of Waterloo. Hana Irving, MA, is the Director, Philanthropic Programs for the Saint Elizabeth Foundation.
Beauty found at the edges: a portrait of community support
By Meghan Sheffield
In the first days of July, there aren’t many flowers blooming, I learned.
I’d sent a text saying “Hello friends, I’m putting out a call for flowers. I went to public school with Kory, the young man who died in downtown Cobourg this week, and though I hadn’t seen him in recent years, I feel the loss of him on a community level, as I imagine you do, too. Some of Kory’s people are gathering tonight in vigil at the bank where he died, and I’m gathering flowers from those of us who have gardens to share with this grieving community. Do you have some blooms in your garden that you’d be willing to share?”
Kory died as a result of a toxic drug poisoning that took his life in the bank vestibule where he was sheltering. His friends were grieving, angry, disbelieving. The wider community was in shock that this could happen here, in such an ordinary place, to a local boy, born and raised.
Those who knew him best, who had been with him in what became his last days and months, began to talk about holding a vigil, a time and place to be together in their grief.
As it turned out, the tulips and peonies had faded and finished, and the dahlias and zinnias hadn’t begun to flourish yet. I got some nervous replies about the current state of the garden. A mom from my daughter’s class texted to say that they were sorry, but just didn’t really have much to offer right now.
Then the first yes rolled in. “Yes, I will pull something together. We have one million daisies.”
A man’s whole life. One million daisies.
As it turned out, there was an abundance to be had, if you knew where to look, if we just widened the margins of “the garden” and looked to the edges of the wild places.
We know that trauma of all kinds is inequitably distributed in our society, and that access to healing resources is even more inequitable. For community members who rely on a prohibited, criminalized supply of certain substances, the experience is not just a risk of personal harm, but of compounding losses and grief. It means mourning in isolation because the cause of death is so stigmatized. It means administering life-saving medicine and performing chest compressions in the glow of flashing lights, while still in mourning for the most recent loss.
I spent an hour driving around, picking up mason jars filled with blooms from doorsteps all over town. There were daylilies and hydrangea, wild vetch and bladderwort, fragrant bee balm and holy basil, and yes, one million daisies.
At the vigil, the jars of flowers were joined by an eagle feather and abalone shell, offerings of cigarettes, and a can of Molson resting on the window sill outside the bank. Candles were lit, stories were told, tears were shed.
Those of us who didn’t know Kory well, who were present to show our support, to acknowledge the community and systemic level failures that had led us to this place, were invited to hold a perimeter of care for those in the centre, who were grieving, by standing at the edges of the gathering.
For days after the sunset vigil, at the doorstep of an ordinary bank, flowers bloomed on the grey cement sidewalk on main street. Wild, fleeting, beauty.
Alongside
By Mike Bonikowsky
Grief is the great leveller, and the great divider. Everyone grieves, sooner or later, but no two people will experience it in the same way. No two bereavements are the same, and neither are any two consolations.
This is only more poignantly the case for people with developmental disabilities. Not only is their grief completely unique, but they are often unable to express it in traditional ways. How are we to support someone through the grieving process when they cannot, or will not, tell us what they are thinking and feeling about their loss? The answer is simple, and difficult.
In Christian theology, there is a concept called “the Holy Spirit”. This is the invisible piece of God that is everywhere all the time, with and within all people. The name given to this in the original ancient Greek is the “Paraclete”, literally, “The one who comes alongside.”
That is also our best, and only role, when supporting a person with a developmental disability to grieve. We must be the one that comes alongside. There is no closer place we can get to. We must be present, be with, perhaps not understanding or comprehending what the person we support is experiencing, but alongside them nonetheless. We must be there, ready to provide whatever we can discover of their unique need in grief.
But that coming alongside must begin before the bereavement. We must already have been there through the happier seasons of the person’s life, if we are to know them well enough to read the language of their grieving, and hope to know in what little ways we may support them. Supporting a person with a developmental disability to grieve is not a matter of coming alongside, but of remaining where we already were. It is a matter of knowing and being known by them, of being trusted. It is not so much a matter of doing anything for the person, but of being something for them: A safe place, a consistent and reliable presence. It is to be a fixed point in a confusing, chaotic world, someone of whom they can say: “When that person is here, I can expect things to be like this.” Only when this relationship is present and well-established in the ordinary times can we come alongside in the darkest, loneliest season on the person’s life, and hope to meet their unspoken needs.
And usually the answer to those needs is what it has always been: To simply be there with them, to prepare a meal for them and do the dishes afterward, to help them wash body and find clean clothes to wear. To open the curtains in the morning, so that when they emerge from the dark cave of their unique grief, for however short a time, they are greeted by a world that has not ended, and a face that they know, and that knows them.
Antoinetta – Grieving in community with others
Antoinetta – Grieving in community with others
Antoinetta discusses how grief camp made her feel so much more happy and how she found support and that she did not feel so alone
What I know about grief
Post by Alyssa Warmland, artist, activist, well-practiced griever.
I earned my “grief card” at 15, when I lost my mother. Since then, I’ve experienced other instances of loss and have become a well-practiced griever. Most recently, I lost a friend in a tragic way. She was deeply connected within our rural Ontario community and as I grieve her loss, I’m watching many other people around me grieve. Some, like me, are experienced in grief. Others are newer to the experience.
The following are some things I know to be true about grief for me, based on my lived experience. Some of them may resonate with you as well. Grief is unique to the people experiencing it in each moment, so please take whatever makes sense to you from this share and leave whatever doesn’t.
– Give yourself space to just feel the waves. Sometimes it feels like it’s not quite so intense, and then sometimes it feels like you’ve just been punched in the stomach. And it’ll cycle around. And it won’t feel this way forever.
– You’re totally allowed to feel whatever it is you’re feeling. Last night, while I spoke with sobbing friends on the phone, I was absolutely furious. Today, it’s that gut-punch feeling. it’ll cycle around. And it won’t be this way forever.
– Sharing stories can be helpful. Celebrate the reasons you loved whoever you’re grieving. Look at the pictures. Watch the videos. Sing the songs.
– Be patient with yourself, but keep going through the motions of what you know you need to do to maintain your wellness while you grieve. Eat something, even if you’re not hungry. Sleep or lay down, even if you feel like you’ll never fall asleep (podcasts can help make it less overwhelming). Drink water. Go for a walk outside. Write about it. Work, if you want to work (and plan for some extensions on stuff if you can, so you can work a bit more slowly than usual if you need to)
– Your brain may take a little longer to process things. Your memory may not work as well. You may feel irritable or overwhelmed. It’s okay.
– If the death part itself was hard, try to avoid focusing on the end, and instead think about the person you loved and who they were when they were well.
– Connect with other people who are grieving, it may be easier to know you’re not alone.
To learn more about collective grief, please read Maureen’s post on the topic.
Collective Grief
Post by Maureen Pollard, MSW, RSW
When the death of a person affects many members in a community, city, country, or across the world, people will experience collective grief.
Some things that can help people through the experience of collective grief across a community include:
– Holding gatherings that allow people share the pain of loss and to remember and honour the person who died;
– Sharing reflective and supportive posts on social media that address the loss and grief being felt by so many;
– It can be helpful to tag the person who died, so it shows up on their page where people can look through for solace. It may be a good idea to avoid tagging the family members of the person who died so that they can
choose when to opt into engaging with these memories without overwhelming notifications;
– Encouraging opportunities for community members to give and receive empathy and compassion;
– Respecting personal differences in the experience and expression of grief among community members, as everyone
grieves in their own way.
While many people across a community may be feeling the loss, it’s important to respect the privacy of those most impacted by the death. Give the immediate family time and privacy. Although many may mourn their loved one, it can be burdensome for the family to have to receive community grief at a time when they are coping with their own grief process.
Donna B – “When risk becomes reality”
Donna B – “When risk becomes reality”
Donna discusses the unlimited liability factor and support. Donna continues to grieve the death her son during service in Afghanistan.
Donna B – “5 Generations of Service”
Donna B – “5 Generations of Service”
Donna talks about her son and how her family understands service. Donna continues to grieve the death her son during service in Afghanistan.
Keith – “Disenfranchised Grief”
Keith – “Disenfranchised Grief”
Keith describes disenfranchised grief.
Amanda – “No person is an island”
Amanda – “No person is an island”
Amanda talks about the power of community and the importance of reaching out.